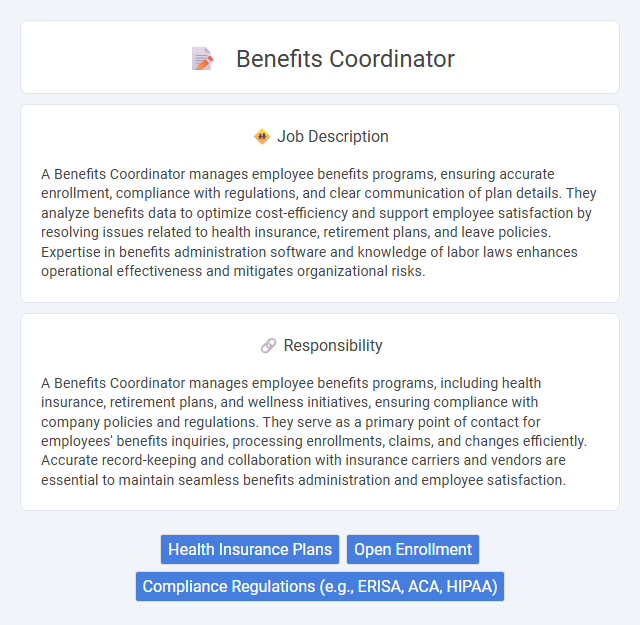
A Benefits Coordinator manages employee benefits programs, ensuring accurate enrollment, compliance with regulations, and clear communication of plan details. They analyze benefits data to optimize cost-efficiency and support employee satisfaction by resolving issues related to health insurance, retirement plans, and leave policies. Expertise in benefits administration software and knowledge of labor laws enhances operational effectiveness and mitigates organizational risks.
People with strong organizational skills and attention to detail are likely to be well-suited for a Benefits Coordinator role. Individuals who thrive in environments requiring clear communication and problem-solving regarding employee benefits may find this position aligns with their strengths. Those who struggle with multitasking or managing confidential information might find the demands of this job less suitable.
Qualification
A Benefits Coordinator must possess strong knowledge of employee benefits programs, including health insurance, retirement plans, and compliance with ERISA and ACA regulations. Proficiency in benefits administration software such as ADP or Workday and excellent communication skills to effectively liaise between employees and insurance providers are essential. A bachelor's degree in human resources, business administration, or a related field, along with relevant certifications like CEBS or SHRM-CP, significantly enhances qualifications.
Responsibility
A Benefits Coordinator manages employee benefits programs, including health insurance, retirement plans, and wellness initiatives, ensuring compliance with company policies and regulations. They serve as a primary point of contact for employees' benefits inquiries, processing enrollments, claims, and changes efficiently. Accurate record-keeping and collaboration with insurance carriers and vendors are essential to maintain seamless benefits administration and employee satisfaction.
Benefit
A Benefits Coordinator likely manages employee benefits programs, ensuring accurate enrollment and compliance with company policies. They probably facilitate communication between employees and benefit providers, which could improve overall satisfaction and understanding of available benefits. Efficient handling of benefits administration may contribute to enhanced employee retention and workplace morale.
Challenge
The Benefits Coordinator role likely involves managing complex employee benefit programs that require attention to detail and problem-solving skills. Navigating diverse insurance plans and compliance regulations may present continuous challenges that demand adaptability and effective communication. The position probably offers opportunities for professional growth by tackling these dynamic and multifaceted responsibilities.
Career Advancement
Benefits Coordinator roles offer substantial opportunities for career advancement through gaining expertise in employee benefits administration, compliance, and vendor management. Mastery of benefits coordination enhances strategic planning skills, positioning professionals for roles such as Benefits Manager or HR Business Partner. Continuous development in benefits analytics and regulatory knowledge further supports progression into senior human resources positions.
Key Terms
Health Insurance Plans
Benefits Coordinators specialize in managing health insurance plans, ensuring employees understand coverage options, premiums, and claims processes. They collaborate with insurance providers to negotiate plan details that optimize cost-efficiency and maximize employee benefits. Their expertise supports compliance with healthcare regulations and enhances overall employee satisfaction through tailored health insurance solutions.
Open Enrollment
Benefits Coordinators play a crucial role in managing Open Enrollment periods by coordinating employee communications and ensuring accurate plan selections. They streamline benefits administration by updating eligibility data, processing enrollments, and resolving coverage issues to maximize employee satisfaction. Effective Benefits Coordinators enhance compliance with regulatory requirements while optimizing benefits utilization and cost-efficiency during Open Enrollment.
Compliance Regulations (e.g., ERISA, ACA, HIPAA)
Benefits Coordinators ensure strict adherence to compliance regulations such as ERISA, ACA, and HIPAA by meticulously managing employee benefits programs and maintaining accurate documentation. Their expertise in federal and state laws helps prevent costly legal penalties and safeguards employee privacy through secure handling of sensitive health information. Staying updated on evolving regulations enables Benefits Coordinators to implement necessary policy changes and foster a compliant, transparent benefits environment.
 kuljobs.com
kuljobs.com