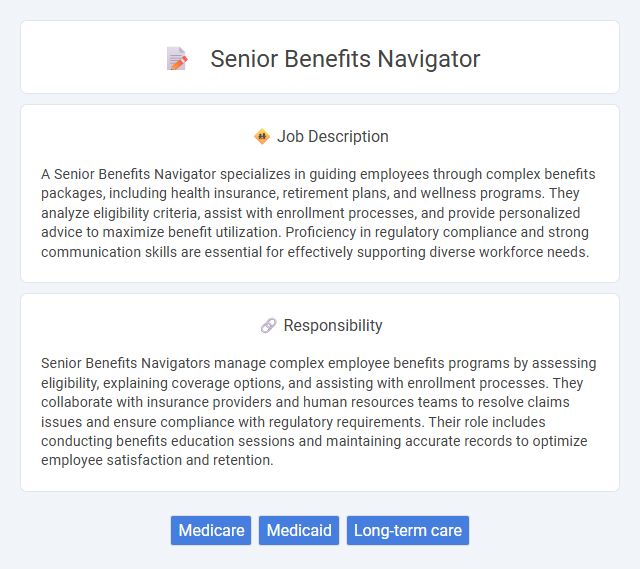
A Senior Benefits Navigator specializes in guiding employees through complex benefits packages, including health insurance, retirement plans, and wellness programs. They analyze eligibility criteria, assist with enrollment processes, and provide personalized advice to maximize benefit utilization. Proficiency in regulatory compliance and strong communication skills are essential for effectively supporting diverse workforce needs.
Individuals with strong communication skills and a compassionate nature are likely well-suited for a Senior Benefits Navigator role, given its focus on helping clients understand and access their benefits. Those who thrive in problem-solving and enjoy working closely with diverse populations may find it rewarding and compatible with their abilities. However, individuals who prefer solitary work or have difficulty managing complex regulations might not find this position as fitting.
Qualification
A Senior Benefits Navigator typically requires extensive knowledge of Medicare, Medicaid, and private insurance plans, alongside strong experience in client counseling and benefits enrollment processes. Advanced degrees or certifications in healthcare administration, social work, or related fields significantly enhance qualification credentials. Proficiency in regulatory compliance, eligibility assessment, and personalized care planning is critical for excelling in this role.
Responsibility
Senior Benefits Navigators manage complex employee benefits programs by assessing eligibility, explaining coverage options, and assisting with enrollment processes. They collaborate with insurance providers and human resources teams to resolve claims issues and ensure compliance with regulatory requirements. Their role includes conducting benefits education sessions and maintaining accurate records to optimize employee satisfaction and retention.
Benefit
A Senior Benefits Navigator likely specializes in guiding individuals through complex benefit programs, ensuring they understand and access the maximum available benefits. They probably evaluate eligibility for various health, retirement, and social security benefits, increasing the probability clients receive the support they qualify for. Their expertise may improve benefit utilization by identifying overlooked resources and providing clear explanations of benefit options.
Challenge
The Senior Benefits Navigator role likely involves navigating complex healthcare systems and insurance policies, which can present significant challenges in staying updated with constantly changing regulations. Probability suggests the position demands strong problem-solving skills to assist clients in understanding and maximizing their benefits. Handling diverse cases and ensuring compliance with legal requirements may also require continuous learning and adaptability.
Career Advancement
A Senior Benefits Navigator role offers significant opportunities for career advancement through developing expertise in employee benefits management and compliance. Mastery in navigating complex benefits plans and counseling employees on healthcare, retirement, and wellness programs positions professionals for leadership roles within HR departments. Continuous learning and certification in benefits administration further enhance promotion prospects and industry recognition.
Key Terms
Medicare
Senior Benefits Navigators specialize in guiding individuals through the complexities of Medicare enrollment, coverage options, and benefits. They provide expert assistance in understanding Medicare Parts A, B, C, and D, ensuring seniors maximize their healthcare benefits and minimize out-of-pocket costs. Their role is critical in helping beneficiaries navigate eligibility criteria, annual enrollment periods, and supplemental coverage decisions.
Medicaid
Senior Benefits Navigators specialize in guiding eligible individuals through the complexities of Medicaid enrollment, ensuring they understand coverage options and application requirements. They assist with verifying income eligibility, explaining benefit packages, and addressing questions related to Medicaid services and renewal processes. Proficiency in state-specific Medicaid policies and strong communication skills are essential for effectively supporting low-income seniors in accessing healthcare benefits.
Long-term care
Senior Benefits Navigator experts specialize in guiding older adults through the complexities of long-term care options, including Medicaid, Medicare Advantage plans, and Veterans Affairs benefits. They offer personalized assessments to determine eligibility for in-home care services, assisted living facilities, and nursing home coverage, maximizing benefit utilization. Their role is critical in helping seniors and their families secure sustainable financial resources and access quality care tailored to chronic health conditions and aging-related needs.
 kuljobs.com
kuljobs.com