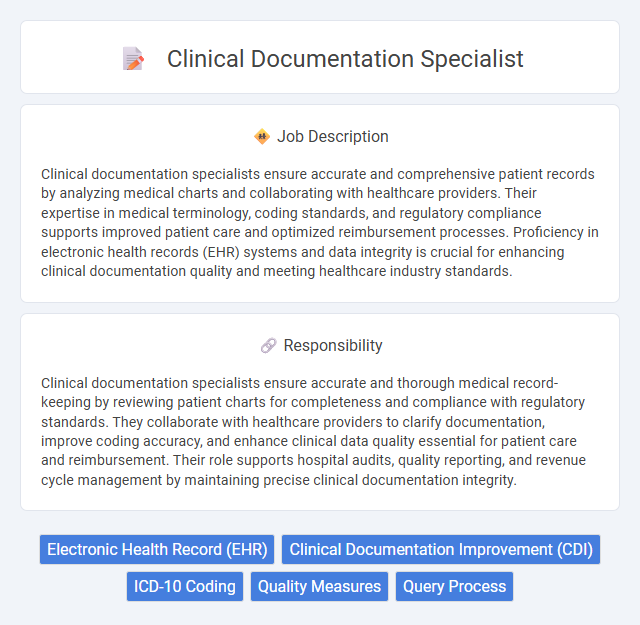
Clinical documentation specialists ensure accurate and comprehensive patient records by analyzing medical charts and collaborating with healthcare providers. Their expertise in medical terminology, coding standards, and regulatory compliance supports improved patient care and optimized reimbursement processes. Proficiency in electronic health records (EHR) systems and data integrity is crucial for enhancing clinical documentation quality and meeting healthcare industry standards.
Individuals with strong attention to detail and a passion for healthcare data management are likely to be well-suited for a Clinical Documentation Specialist role. Those who can thrive in fast-paced environments and possess excellent communication skills may have a higher probability of success in accurately capturing patient information. People who find repetitive tasks challenging or struggle with medical terminology might face difficulties in this position.
Qualification
Clinical documentation specialists require a background in healthcare, often holding a nursing degree or allied health certification combined with expertise in medical terminology and coding systems like ICD-10 and CPT. Proficiency in electronic health records (EHR) software and strong analytical skills are essential for accurate data interpretation and improving clinical documentation quality. Certifications such as Certified Clinical Documentation Specialist (CCDS) enhance job prospects by validating specialized knowledge in documentation improvement and compliance standards.
Responsibility
Clinical documentation specialists ensure accurate and thorough medical record-keeping by reviewing patient charts for completeness and compliance with regulatory standards. They collaborate with healthcare providers to clarify documentation, improve coding accuracy, and enhance clinical data quality essential for patient care and reimbursement. Their role supports hospital audits, quality reporting, and revenue cycle management by maintaining precise clinical documentation integrity.
Benefit
A Clinical Documentation Specialist likely enhances the accuracy and completeness of patient medical records, which may lead to improved patient care and insurance reimbursement. This role could reduce the risk of compliance issues and support better communication among healthcare providers. Professionals in this position might also experience increased job stability and opportunities for career advancement within healthcare organizations.
Challenge
Clinical documentation specialists likely encounter considerable challenges ensuring accuracy and completeness in medical records, which is crucial for patient care quality and compliance with healthcare regulations. They probably face difficulties reconciling discrepancies between clinicians' notes and coding requirements, requiring a deep understanding of both clinical terminology and regulatory standards. Managing time effectively amidst evolving documentation guidelines and electronic health record systems may also present ongoing obstacles.
Career Advancement
Clinical documentation specialists play a crucial role in ensuring accurate and comprehensive medical records, directly impacting patient care quality and hospital reimbursement rates. Career advancement opportunities include moving into managerial positions, health information management leadership roles, or specialized consulting, often requiring certifications such as Certified Clinical Documentation Specialist (CCDS). Expertise in medical terminology, coding systems like ICD-10, and electronic health records (EHR) systems enhances prospects for promotion and salary growth within healthcare organizations.
Key Terms
Electronic Health Record (EHR)
A Clinical Documentation Specialist ensures accuracy and completeness of patient information within Electronic Health Record (EHR) systems, optimizing healthcare data quality for improved patient outcomes. They analyze clinical notes, collaborate with providers, and implement documentation best practices to enhance coding and billing processes. Expertise in EHR software like Epic or Cerner is critical for streamlining workflows and supporting compliance with regulatory standards such as HIPAA.
Clinical Documentation Improvement (CDI)
Clinical Documentation Specialists play a critical role in Clinical Documentation Improvement (CDI) by ensuring medical records accurately reflect patient diagnoses, treatments, and outcomes to enhance healthcare quality and reimbursement accuracy. They collaborate with physicians, coding staff, and quality teams to identify documentation gaps, clarify clinical language, and support compliance with regulatory standards such as ICD-10 and HIPAA. Expertise in clinical terminology, healthcare regulations, and data analytics is essential for optimizing CDI processes and improving patient care documentation integrity.
ICD-10 Coding
Clinical Documentation Specialists play a critical role in healthcare by ensuring accurate and complete patient records through expert ICD-10 coding. They analyze medical records to extract detailed diagnostic and procedural information, enhancing code specificity and compliance with coding standards. Proficiency in ICD-10 coding improves reimbursement accuracy, supports quality reporting initiatives, and reduces the risk of audits or claim denials.
Quality Measures
Clinical documentation specialists play a critical role in ensuring accurate and comprehensive medical records that directly impact quality measures used by healthcare organizations. They analyze documentation to support compliance with regulatory standards such as HEDIS, CMS quality initiatives, and Joint Commission requirements, which enhances patient care outcomes and reimbursement accuracy. Their expertise in coding, clinical terminology, and cross-departmental collaboration improves data integrity, facilitating better performance tracking and quality improvement efforts.
Query Process
Clinical documentation specialists enhance healthcare quality by optimizing patient records through an effective query process. Their role involves analyzing medical charts and collaborating with providers to clarify documentation ambiguities, ensuring accurate diagnosis and treatment coding. This targeted querying supports compliance, improves reimbursement accuracy, and promotes better clinical decision-making.
 kuljobs.com
kuljobs.com